Non-Emergency Medical Transportation (NEMT)
Solutions for health plans, state agencies, and transportation providers

What is NEMT and why it matters
Non-Emergency Medical Transportation (NEMT) ensures Medicaid members can access care when they do not require an ambulance. For health plans, state agencies, and transportation providers, NEMT is more than a transportation service. It is a federally mandated benefit and an essential part of equitable care delivery. Medicaid requires states to ensure transportation access for eligible members under federal NEMT guidance from CMS.
Missed trips or denied claims affect member health, compliance, and performance metrics. Inefficient NEMT programs can increase costs and create administrative burden. Leading Medicaid managed care organizations (MCOs) and transportation networks are turning to digital platforms that improve efficiency, visibility, and accountability across every ride.
Why NEMT matters for health plans and state agencies
Under Medicaid, NEMT is a required benefit to ensure members can reach essential medical appointments. For health plans and state agencies administering Medicaid transportation programs, NEMT is not only a compliance requirement but also an opportunity to improve outcomes and manage costs.
Effective NEMT programs can:
- Reduce overall cost of care by improving access to preventive and routine services.
- Strengthen compliance with federal and state transportation mandates.
- Improve performance metrics and member satisfaction.
- Support health equity by removing transportation barriers.
Challenges for transportation providers
Transportation providers working within Medicaid networks manage complex operations that vary across payers and states. Common challenges include:
- Manual billing processes and delayed payments.
- Difficulty optimizing routes and schedules.
- Missed reimbursements due to documentation errors.
- Varying compliance standards and reporting requirements.

Billing and revenue cycle
Accurate billing is essential to financial stability. NEMT billing software can streamline every stage of the revenue cycle, from trip authorization and claim submission to reconciliation and reporting. Automation reduces denials, accelerates reimbursement, and ensures alignment with Medicaid billing standards. For organizations operating across multiple states, centralized revenue cycle management provides visibility and control across all programs.

Operational inefficiencies
Manual scheduling and outdated systems make it difficult for transportation providers to operate efficiently. Without centralized visibility, dispatch teams spend valuable time managing calls, spreadsheets, and overlapping routes.
NEMT dispatch software gives providers real-time control over trip assignments, routing, and vehicle utilization. Integrated trip verification ensures every ride is logged accurately, reducing billing disputes and improving on-time performance.
By connecting dispatch, billing, and reporting into one platform, Kinetik helps providers eliminate redundant processes, reduce administrative effort, and deliver a better experience for members and drivers alike.
Navigating the regulatory landscape
Medicaid NEMT compliance is shaped by both federal CMS guidance and state-specific regulations. Health plans, MCOs, and transportation providers must work together to ensure accurate documentation, fraud prevention, and transparent reporting. Industry resources such as NEMTAC and The Medical Transportation Access Coalition (MTAC) provide operational best practices and safety standards.
Key requirements include:
- Verified member eligibility and trip authorization.
- GPS-based trip validation.
- Fraud, waste, and abuse prevention controls.
- Audit-ready documentation and reporting.
Kinetik simplifies Medicaid NEMT compliance with configurable workflows, automated documentation, and state-level reporting capabilities that reduce administrative risk.
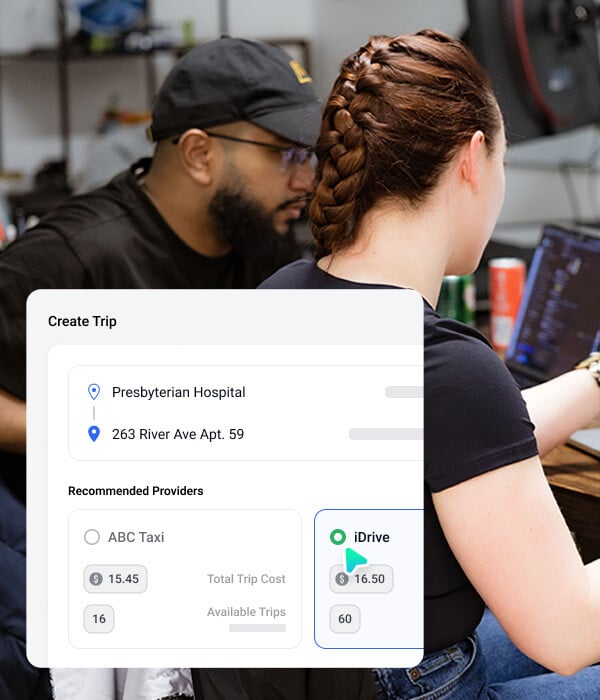
Technology’s role in modernizing Medicaid NEMT
Traditional NEMT operations often rely on manual coordination or third-party brokers that limit visibility. A modern technology platform provides efficiency, transparency, and control. Kinetik’s NEMT platform gives health plans, MCOs, and transportation providers the ability to automate workflows, track compliance in real time, connect dispatch and billing systems, and use analytics to improve performance.
The future of Medicaid NEMT
As Medicaid programs expand their focus on health equity and value-based care, transportation plays a critical role in addressing social determinants of health. For more background on SDoH, visit the CDC’s Social Determinants of Health resource.
Reliable NEMT helps members access preventive, behavioral, and chronic care services that improve outcomes and reduce costs. The future of NEMT will rely on better data, stronger coordination, and technology that connects health plans, providers, and members in one transparent system.
Why Kinetik
Stay compliant with CMS and state Medicaid transportation rules.
Simplify billing and revenue cycle management for providers.
Improve operational efficiency and reporting accuracy.
Build transparency and trust among members and partners.
Kinetik connects health plans, Medicaid managed care organizations, state agencies, and transportation providers on one unified NEMT platform. Unlike traditional brokers or service vendors, Kinetik’s technology-first approach combines automation, analytics, and compliance capabilities to strengthen Medicaid transportation programs.
Stay compliant with CMS and state Medicaid transportation rules.
Simplify billing and revenue cycle management for providers.
Improve operational efficiency and reporting accuracy.
Build transparency and trust among members and partners.
Frequently asked questions about NEMT
What is Non-Emergency Medical Transportation (NEMT)?
NEMT provides transportation for Medicaid members who need access to healthcare services but do not require an ambulance. These rides are essential to connecting members to primary and preventive care. For health plans, state agencies, and providers, NEMT is both a compliance obligation and a vital part of member care.
Why is NEMT important for Medicaid programs?
Under Medicaid, NEMT is a federally required benefit that ensures members can reach covered healthcare services. While the term “non-emergency” can be misleading, these rides are often critical to maintaining continuity of care helping members access dialysis, chemotherapy, behavioral health, prenatal visits, and other essential appointments.
For health plans and Medicaid managed care organizations, effective NEMT management reduces avoidable emergency visits, supports compliance with state and federal requirements, and improves quality measures related to access and outcomes.
How does NEMT billing software help providers?
NEMT billing software streamlines every step of the revenue cycle from trip documentation and claim submission to reconciliation and reporting. Automated billing reduces denials, accelerates reimbursement, and ensures compliance with Medicaid requirements.
For transportation providers operating across multiple states and contracts, centralized revenue cycle management tools provide the visibility needed to track claims, prevent revenue leakage, and sustain financial performance.
How do health plans and MCOs stay compliant with Medicaid NEMT requirements?
Compliance requires accurate eligibility checks, documented ride data, fraud prevention controls, and detailed state-level reporting. Modern NEMT platforms provide audit-ready transparency while reducing the administrative burden for health plans and transportation networks.
What role does technology play in NEMT?
Technology transforms NEMT from a fragmented, manual process into an integrated system. With real-time ride tracking, automated billing, and robust data analytics, health plans and providers gain the visibility and accountability they need to improve efficiency and member outcomes.


